What we learnt from our Social Prescribing Pilot Program

Welcome to IPC Health's Social Prescribing Pilot Program summary. Learn how our program has enhanced lives and reduced healthcare burden in Melbourne's western region.

About IPC Health
IPC Health is a not-for-profit community health centre based in Victoria, Australia that bridges primary and tertiary care. With six sites across Melbourne’s western region, our 550+ staff deliver integrated medical, dental, mental health, and social services. We’re dedicated to providing client-centred care that has a real, measurable impact on our diverse, fast growing community.

What is social prescribing at IPC Health?
Social prescribing is a person-centred model of care that complements traditional healthcare by addressing social and emotional wellbeing. It links individuals with non-medical support services to reduce loneliness, increase confidence, and build meaningful social connections. Our Social Prescribing Pilot Program, which ran from 2019 to 2022 in Brimbank and Wyndham, provided support to individuals referred by GPs and other health providers. Wellbeing Coordinators worked with clients to assess their needs, create tailored care plans, and connect them with local services and activities.
Evaluation overview
The program evaluation, conducted from April 2021 to September 2022, explored its impact on clients' quality of life and the healthcare system. Supported by the North Western Melbourne Primary Health Network and led by IPC Health, the evaluation included client surveys, program documentation, and input from our Social Prescribing team. Consultant Anna Vu supported us in the full evaluation report.

Our purpose is to improve quality of life for the people and communities we serve by maximising access to health and wellbeing services.
Key Findings
Addressing holistic needs
The program focused on assessing and addressing the full range of social, physical, and mental health needs of clients.
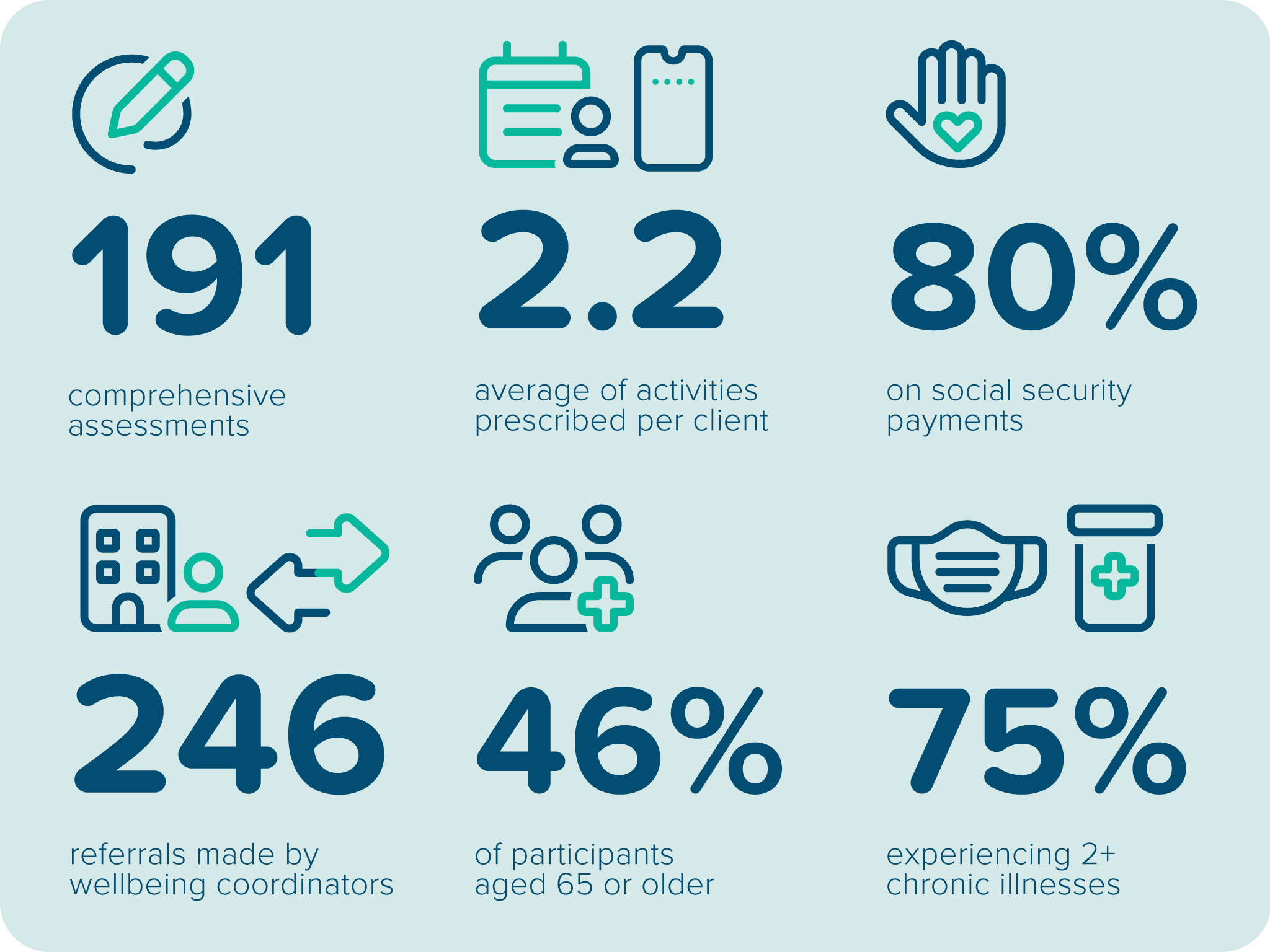
- 191 clients received comprehensive assessments of their social, physical, and mental health needs
- Our multidisciplinary Wellbeing Coordinators made 246 referrals, prescribing an average of 2.2 social activities per client
- The model identified unmet needs and connected clients to appropriate services
Reaching populations in need
The program successfully reached marginalised and vulnerable groups, particularly older adults and those facing social and health challenges.
- 46% of clients were aged 65 or older
- 80% were on social security payments, and 75% experiencing two or more chronic illnesses
- Clients faced social disadvantages like food insecurity, mental illness, or chronic pain
Positive impact on wellbeing and healthcare use
The program not only improved clients' overall wellbeing but also reduced their need for medical services, easing the burden on healthcare systems.
- Clients reported improvements in mental, physical health, and reduced loneliness
- The program led to fewer GP visits, fewer emergency department presentations, and reduced unplanned hospital stays
Conclusion and recommendations
A proven approach
Our social prescribing pilot has shown that addressing social and clinical needs holistically enhances wellbeing and reduces pressure on healthcare services. By integrating Wellbeing Coordinators and a broad range of support services, IPC Health has helped improve clients' quality of life while easing the burden on medical systems.
Recommendations
For funders:
- Support community health services as optimal environments for social prescribing
- Provide sustainable funding to integrate Wellbeing Coordinators into healthcare teams
- Ensure adequate resources for social activities and maintain an updated directory of programs
For future programs:
- Design flexible, holistic support systems
- Employ Wellbeing Coordinators skilled in clinical care, empathy, and service navigation
- Leverage community resources, including volunteer or peer support, to enhance program effectiveness
- Take the time to collect data so you can refine and expand program impact






Want to learn more?
For detailed insights, download our summary of the Social Prescribing Pilot Program or get in touch with us at socialprescribing@ipchealth.com.au to request the full report.