


The 2020–2021 financial year will always be defined by COVID-19 and our agility, resourcefulness and resilience in responding to a global pandemic. Everyone at IPC Health has worked above and beyond to contribute to the year’s achievements. We are very proud to be able to present them to you in this year’s Annual Report.

IPC Health has continued with its growth and leadership trajectory in the community health sector with our COVID-19 response, working closely with the Commonwealth and State Departments of Health, hospitals and other community health organisations across metro Melbourne to deliver Acute Respiratory Clinics (ARC), Rapid Response COVID-19 Testing, Community Engagement and COVID-19 Vaccinations. Our COVID-19 Response is inclusive of a bicultural workforce that connects with local communities to educate, prevent transmission and encourage vaccinations in an effort to keep our local communities safe.
Our focus has remained on connecting clients with much needed care, providing culturally appropriate access to services for those who do not always feel comfortable approaching mainstream health, and supporting our local communities.
IPC Health staff have continued to deliver services, often in creative and innovative ways given the pandemic restrictions. They are a testament to IPC Health’s overall achievements this year. We would like to thank all our staff who have demonstrated passion, commitment and resilience in challenging circumstances to make a difference for those most in need.
IPC Health’s Strategy to 2025 focuses on deeply understanding our diverse community, providing exceptional health and wellbeing services, prevention of poor health outcomes, and improving people’s quality of life. In 2020–2021 IPC Health expanded much needed mental health services by launching the IPC Health HeadtoHelp Hub in Wyndham in partnership with the North Western Melbourne Primary Health Network (NWMPHN). The Hub is now being expanded to include Melton in partnership with Melton City Council and demonstrates our commitment to working with the rapidly growing areas of Melbourne’s middle and outer West.
During COVID-19 our focus has always been to keep our clients and staff safe while continuing to provide services. IPC Health invested in our Modern Workplace project for staff that has seen an overhaul of our information technology systems, telephony platform, and purchase of new mobile equipment delivering the capability for staff to work offsite in real time, supplying services where they are needed.
IPC Health secured new partnerships in 2020–2021 including working closely with the Murdoch Child Research Institute investigating a Child and Family Hub in Wyndham to engage families, better detect and address adversity, and deliver evidence-based holistic care. IPC Health has also partnered with Movember and Hope Assisted Local Tradies (HALT), securing funding to produce a mental health and wellbeing check-in app for tradies and blue-collar workers. Our positive outcomes and impact with our Social Prescribing program continues to gain media recognition, securing additional funding from the NWMPHN and allowing for the expansion of services from Brimbank to include Wyndham.
IPC Health welcomed Ngaire Anderson as a new Board Director in March 2021. We would like to acknowledge and thank our Board Director Rennis Witham who retired from the IPC Health Board in early July 2021 after more than five years of service. Rennis chaired the IPC Health Clinical Governance and Clinical Risk Committee since its inception and her contribution to IPC Health and more broadly to community health has been greatly valued.
IPC Health has achieved a positive surplus of $5.18m for 2020–2021 and while we were unable to deliver all our contracted service hours due to COVID-19 restrictions, we were able to offset the shortfall in service delivery by providing our COVID-19 response, including Acute Respiratory Clinics, pop up drive through testing clinics, mobile testing teams, health status stations, and pop up COVID-19 vaccinations services.
Any surplus generated by IPC Health, known by our staff as surplus for purpose, is invested back into our organisation through expansion of much needed services for our local communities, such as asylum seeker medical and resettlement assistance and dental services in Wyndham. Other surplus funds are directed to supporting our staff Innovation Challenges, developing ideas and new services through a co-design framework with clients, community representatives, peak bodies and partners. Current Innovation Challenges include our Power Over Pain partnership with Western Health; exploration of the delivery of safe and inclusive services and support for transgender, gender diverse, and non-binary people; and exploration of the availability of eating disorder services and support across the western region of Melbourne.
We have driven and pursued opportunities for IPC Health to secure additional program funding to the value of $27.7 million including additional funding for our COVID-19 response such as testing, engagement, High Risk Accommodation Response, Social Prescribing and mental health.
Data from our online Client Feedback Survey show that our clients’ overall satisfaction and experience with IPC Health continues to be very positive: a total of 96% of surveyed people told us they were happy or very happy with the service and 90% were likely or extremely likely to recommend us to their friends and family. Data from our online telehealth survey show 97% of surveyed people were happy or very happy with the service they received and 84% were likely or extremely likely to recommend us.
We would like to thank all Board Directors, Executive and Leadership Teams, staff and volunteers for their excellent work in very challenging times. We would not have been able to deliver our achievements without your ongoing support. We are One Team IPC Health, we are passionate, creative and together, we make a difference.

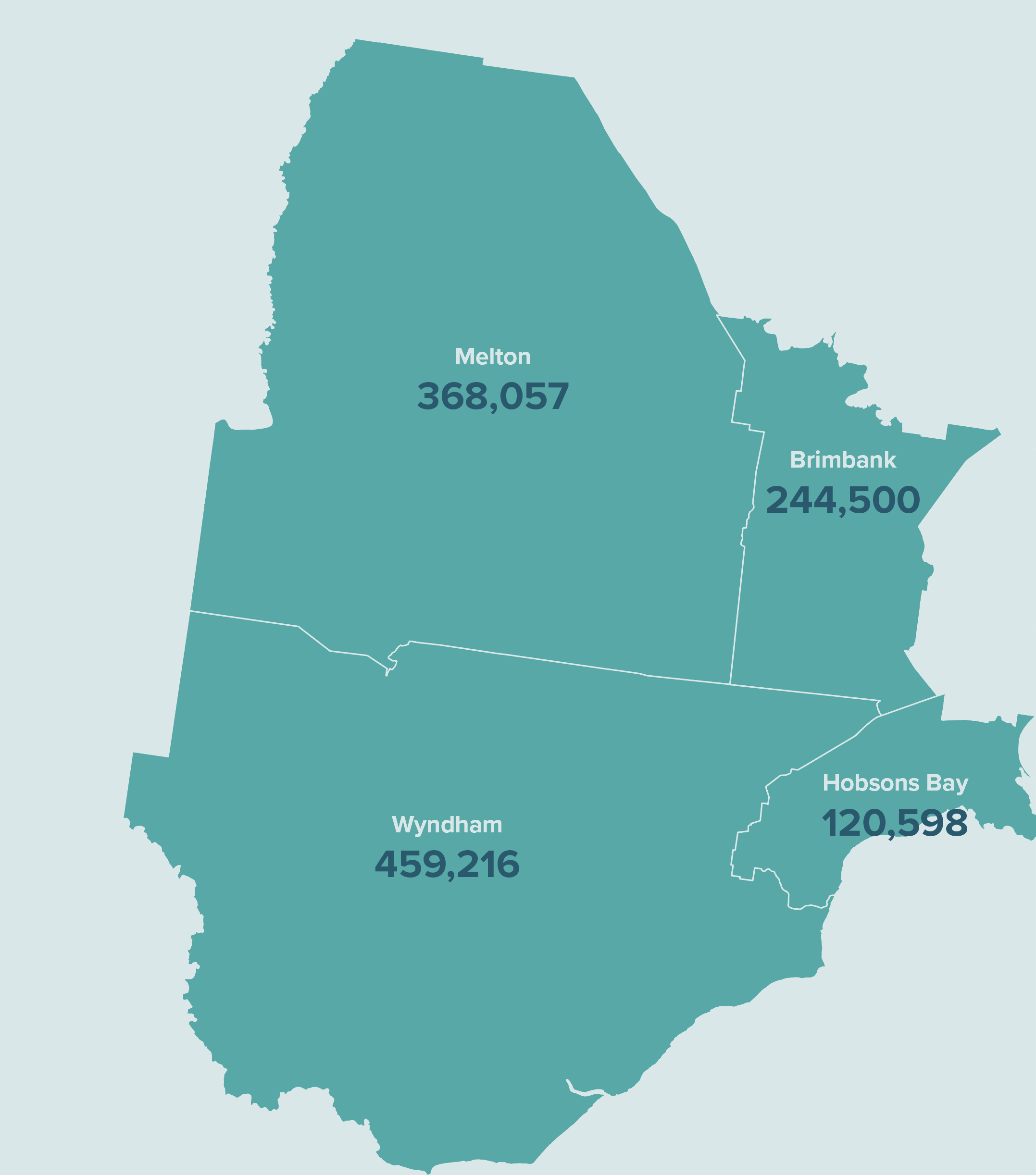
IPC Health is committed to working with the rapidly growing areas of Melbourne’s middle and outer West, where the population will grow by 400,000 in the coming 15 years. By the year 2035, the total population we serve is forecast to grow to approximately 1.2 million.
Aged care
Allied health
Child, youth and family
Chronic conditions
COVID-19 testing and vaccination
General health
Wellbeing and counselling


Source: IPC Health telehealth surveys July 2020 – December 2020
of surveyed telehealth clients told us they were happy/very happy with the service received
of surveyed telehealth clients were likely/extremely likely to recommend IPC Health to family and friends
Source: IPC Health client surveys November 2020 – June 2021
of surveyed telehealth clients told us they were happy/very happy with the service received
of surveyed telehealth clients were likely/extremely likely to recommend IPC Health to family and friends
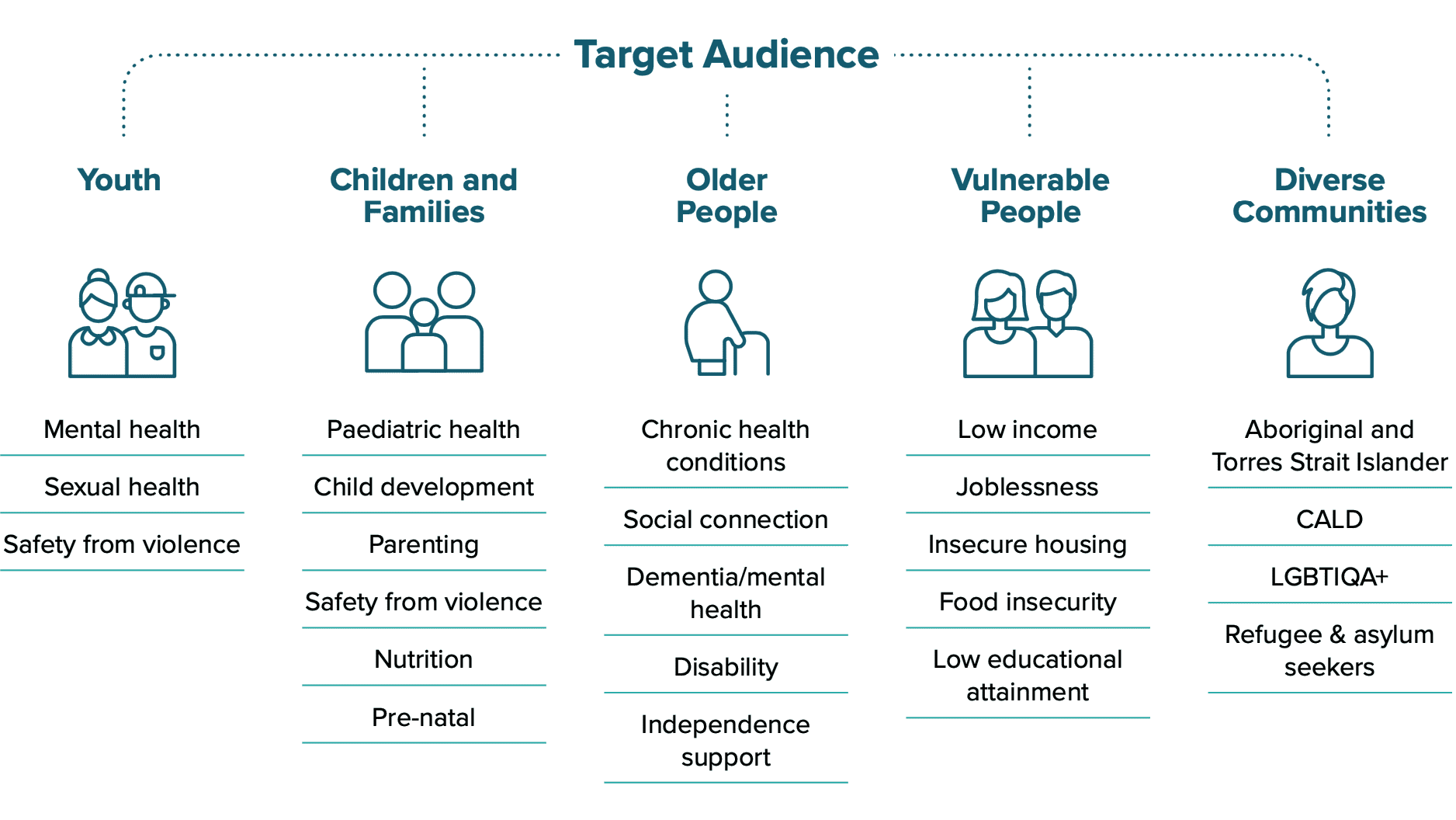
IPC Health’s strategy to 2025 articulates our aim to become a client centred, innovative and responsive organisation that improves quality of life for the people and communities we serve.
Our mission is to deliver innovative high-quality services that are client centred, collaborative, coordinated and demonstrate value through measured impact. We are One Team working together with passion and creativity to make a difference to our local communities.


As part of our IPC Health Strategy to 2025, we intend to invest in the expansion of services most needed by our local communities or in innovative solutions to address key service gaps.
We’re calling this surplus for purpose, where a portion of generated surplus is allocated to areas nominated by our staff and supported by the Executive Leadership Team and IPC Health Board.
This year our surplus for purpose funding was used to:

IPC Health staff from the Social Prescribing and Counselling programs have been assisting me with the management of chronic pain and I am challenged to find the words that convey my appreciation for their support.
I was invited to participate in virtual reality (VR) technology that was being trialled. The experience was most rewarding and the knowledge that I have gained in regards to the mechanisms of pain and the role our brain plays in the pain/brain connection has changed the way I view and manage my pain. At first I was a little sceptical but my scepticism was soon replaced with enthusiasm by the conclusion of my first VR session. I was able to comprehend the brain/pain connection: in simplistic terminology the brain can be distracted from its focus/ connection to a damaged body part. And based on my VR experience I absolutely believe this technology has a valuable role in pain management
I am now aware that my constant battle against pain was in fact counterproductive. I now acknowledge the pain as something that has come to live with me. I now focus on how to distract the brain/pain connection. I have found being productive is crucial in this quest. Virtual reality technology proves this point: your mind/brain is busy, its focus is on something that requires conscious input, and for me that assists with living with chronic pain. The brain/pain relationship is paramount to our wellbeing, if we allow the brain/pain connection to become overly active, it then has the potential to be detrimental to a healthy and productive life.

Moving from treatment to prevention is imperative to ensure we are making improvement to the quality of life for our communities across Melbourne’s west.
Read more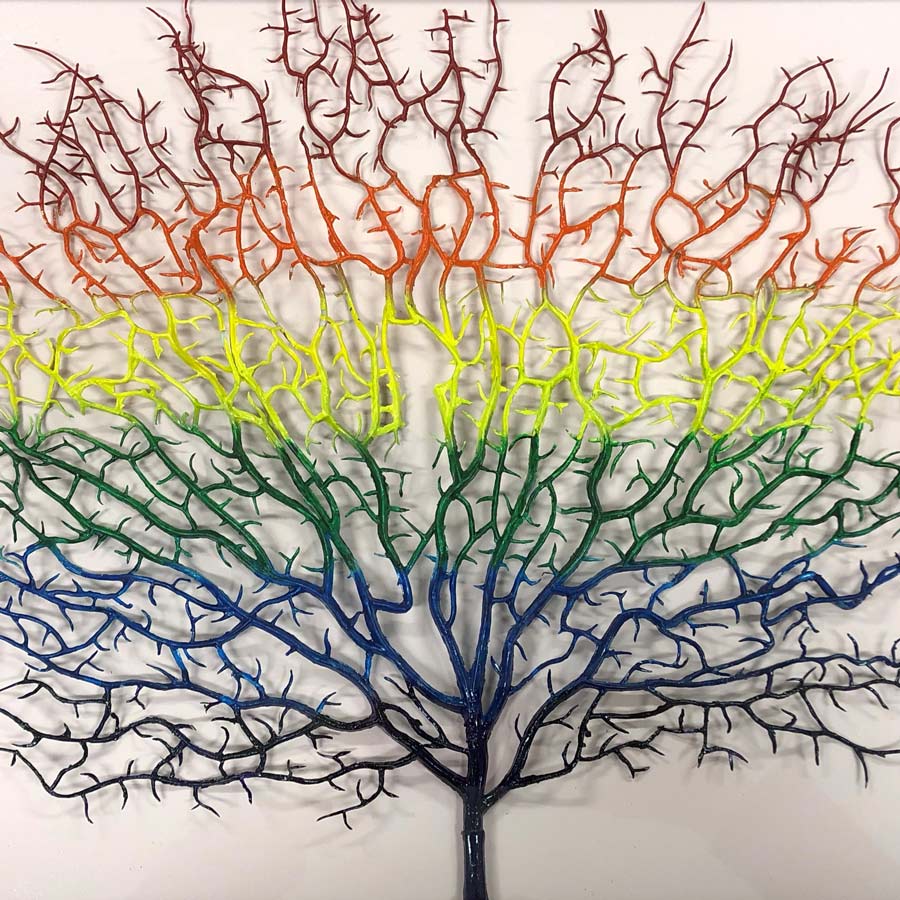
We were honoured to have Uncle Gary Davidson (Taungurung) create a special art piece for our LGBTIQ+ community. We look forward to coming together for an official recognition ceremony once restrictions have eased.
"My artwork piece represents the colours of the LGBTIQ+ community. It’s symbol to me is a tree of life and recognises the struggle that the community are faced with at times. I have family and friends that are proud to be in this LGBTIQ+ community, and for this reason, I have put my mind to making this art piece with great pleasure."
Working together with Brimbank, Hobsons Bay, Melton and Wyndham City Councils and the Queer Youth Alliance Network (QYAN), the Sex Positivity and Rainbow Youth Project collaborates with LGBTIQ+ young people to help them create a safe and positive culture in order to improve their mental health.

IPC Health was one of the first organisations to establish drive through Acute Respiratory Clinics and mobile pop up testing sites at the beginning of the COVID-19 pandemic. We have continued to lead the way with our creativity and responsiveness to the needs of the community across Victoria.


When the Department of Health published a tender for the establishment of COVID-19 Rapid Response Testing Teams (RRTT), a group of likeminded community health organisations banded together to submit a joint submission in the four day timeframe. The successful submission was the beginning of a collaboration between five community health organisations (IPC Health as lead agency, Star Health, DPV Health, cohealth, EACH) forming the C-19 Network to pool resources and expertise as metropolitan and state wide responders to the COVID-19 outbreaks. Between us we have grown to 12 Rapid Response Testing Teams along with a community engagement and bicultural officer workforce who respond 7 days a week to outbreaks anywhere across metropolitan Melbourne.
As lead agency, a central Operational Support Team has been established at IPC Health. The Operational Support Team provides a point of contact for the Department of Health and is the conduit to allocate testing and engagement assignments with our partner organisations.
Rapid Response Testing Teams
The C-19 Network also played a key role in establishing COVID-19 testing services that are able to be rapidly mobilised and establish safe and operations in multiple contexts. From high throughput pop up sites to complex residential and bespoke in home testing services; from skate parks to shopping centres; ports of entry to airline staff quarantine hotels; large apartment blocks to private households; and workplaces to places of worship, wherever testing has been required, the C-19 Network testing teams have delivered. We have an effective capability to engage with at-risk and vulnerable communities, delivering caring, safe and effective testing services in the most high-risk of settings. As of June 2021, the C-19 Network had collectively tested over 300,000 people across the five partner organisations. The Network achieved this without a single transmission of the virus to staff members.
Some highlights:
The team was called on to work in conjunction with the renowned Peter Doherty Institute and the Victorian Infectious Diseases Reference Laboratory as well as Victoria Police in a COVID-19 saliva test implementation pilot rolled out in large workplace settings.
The C-19 Network was part of the response to the Kings Park complex outbreak, establishing and running a pop-up clinic in Sturt St, Southbank for two weeks. This undertaking was a huge logistical exercise and the C-19 team did an amazing job in delivering high level planning, holding partner briefings, continual liaison with the Department of Health and onsite contacts as well as onsite team support. Almost 200 individuals were tested which was the biggest in-home testing exercise ever requested of a public health unit and it was wholly conducted by C-19 Network’s Rapid Response Testing Teams.
Similarly at another Southbank apartment tower, the IPC Health testing teams performed in-home testing for potential and confirmed cases as well as close contacts where they were the only team to include serology (blood testing).
Rapid Response Community Engagement
Our Rapid Response Community Engagement Teams have been fundamental to the success of the C-19 Network’s program. Effective engagement is the primary driver of maximising participation in testing and spreading the message on COVID safe behaviours. Their role is one
of community engagement, COVID-19 safety education, and community support. They specialise in engaging with culturally and linguistically diverse communities, including in high risk work and accommodation settings, who are experiencing barriers to COVIDSafe messaging They are also deployed in support response to emerging COVID-19 cases, clusters and outbreaks. You may have seen them at the Boxing Day Test or Australian Open.
Bicultural Officer Workforce
The Bicultural Workers are employed to establish relationships and deepen connections with individuals and communities with whom they share similar cultural experiences and understanding. They share COVIDSafe information and messaging with communities via effective consultation, in relevant languages and culturally appropriate ways. They also provide additional levels of support for individuals, families and households who might need to go into mandatory quarantining after COVID-19 testing. As role models for their local communities, they (and we) are proud of the work they do to help keep Victoria safe.

Rapid Response Testing Teams
Acute Respiratory Clinic
Existing IPC Health staff seconded
Agency staff used
Newly hired staff
Agency staff now employed by IPC Health
Vaccinations given by IPC Health through the C-19 Network
Vaccinations given in total by all C-19 Network partners


Our High Risk Accommodation Response team have been providing masks, hand sanitiser, and health information in multiple languages to people living in public and community housing, rooming houses, caravan parks, supported residential services and residential disability settings.
We set up concierge stations to help residents get what they needed to stay safe while isolating or quarantining; we also provide COVID-19 testing onsite.
During these times the team encountered residents experiencing incredible isolation, disconnection and hardships as well as some with challenging and complex needs. Most of the residents hadn’t had support from any services for a long time. The Health Concierge was able to link residents with much needed services including housing, health, mental health, tenancy support services, emergency relief and material aid, community programs, and training and employment opportunities.
The Health Concierge team met one person who had been sleeping on the floor for several months as they didn’t have a bed or furniture. They didn’t know where to go to for support and found it hard to access services because of a broken phone. The team were able to source a bed, linen, pillow and quilt, a reclining lounge chair, and food vouchers through the Salvos Hobsons Bay. The team also helped to get the phone working again.
One of the residents said that through their involvement with IPC Health, they now have hope. Another resident has taken to occasionally cooking lunch for the Health Concierge staff as a way of saying thanks and the team says the food is fabulous.

Health Concierge staff provided and/or facilitated pathways for:
Rapid Response Community Engagement and Bicultural Workforce
Our Rapid Response Community Engagement Team and Bicultural Workforce have been proudly working to keep the Victoria public informed about COVIDSafe practices. They actively engage culturally and linguistically diverse communities who otherwise find the mainstream
Following our successful community engagement at Quang Minh Temple last December for the New Moon prayer day, the Rapid Response Community Engagement and Bicultural Workforce team were invited by the Temple’s Abbot to attend their Lunar New Year Festival. Their presence provided great support to the Vietnamese Buddhist community and particularly the Temple. Disposable and reusable masks were distributed along with flyers in both English and Vietnamese. Hand sanitisers were also placed at different locations around the Temple for easy accessibility. In addition to promoting COVIDSafe practices and the importance of testing, the team also discussed the upcoming rollout of the vaccine with the Temple’s committee and members of the Vietnamese community. The Abbot sent us an official email and messages to thank us for our contribution to the Temple’s largest annual event.

A couple of our Bicultural Workers got to be in the vaccine spotlight when the LOTE Agency asked if they could film them receiving their jabs. The LOTE Agency is contracted by the Department of Health to support culturally and linguistically diverse community communications. The footage was used as a resource in the LOTE Agency stakeholder communications pack and shared nationally with community groups.

Our Community Health Champions program is proudly community led. It supports members of culturally and linguistically diverse communities to develop and deliver COVID-19 education and awareness raising activities relevant to the needs of their communities.
With funding from the Department of Premier and Cabinet, and in collaboration with the Local Area Partnerships
in Brimbank and Wyndham, 39 community members representing 13 language groups hosted over 30 different events reaching more than 7000 community members.
These sessions improved community understanding and awareness around the pandemic and increased their access to support services, provided peer and leadership connections while enabling communities to stay up to date with the latest information in their own languages.
The work continues, and thanks to feedback from our communities, we’re pleased to have integrated a Nurse Educator into the program to help deliver information sessions on the vaccine roll out and COVID-19 infection control where requested.


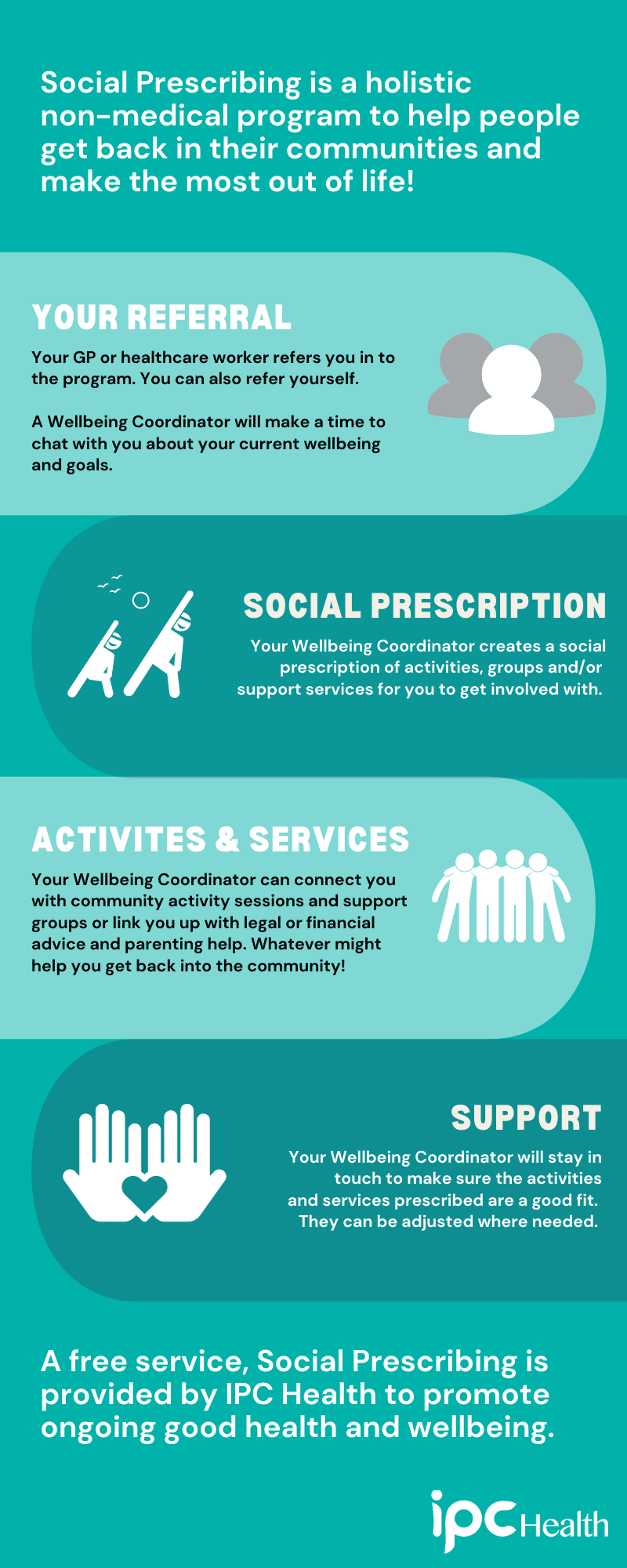
IPC Health has extended our Brimbank based Social Prescribing pilot program into Wyndham with a multidisciplinary team of six wellbeing coordinators. This has been made possible through funding partners at the North West Melbourne Primary Healthcare Network (NWMPHN).
Social Prescribing is a person-centred program that looks to improve a client’s overall wellbeing in non-medical ways in conjunction with their GP or healthcare worker.
A social prescription can complement traditional forms of healthcare by connecting people with activities and services within their local communities that protect and promote health and wellbeing, such as exercise groups, parenting support, legal and financial advice. Wellbeing coordinators are now working across a number of our other programs, such as HeadtoHelp and Power Over Pain, integrating a holistic approach into clinical service delivery to bolster client outcomes.
Unfortunately, multiple hard lockdowns during the COVID-19 pandemic forced the closure of non-essential services as well as planned activity and social groups which limited options for clients to fulfil their social prescriptions. Despite this, we have supported 164 clients through the 2020–2021 financial year, with a total of 477 referrals from June 2019 to July 2021. Currently, 80% of clients with a wellbeing plan are waiting to commence their social prescriptions.
Together with the NWMPHN, we aim to collect patient reported health outcome and experience measures to improve evidence of the effectiveness of social prescribing services within an Australian context. We continue to share our learnings with others and have been pleased to present on our Social Prescribing program and experiences at multiple forums including Mental Health Australia, Consumers Health Forum of Australia, the University of Melbourne and the Western Melbourne Integrated Care Community of Practice.
To respond directly to the significant impact the pandemic is having on the mental health of individuals and communities, we opened the IPC Health HeadtoHelp Hub based at our Wyndham Vale campus in September 2020. Funded through the North Western Melbourne Primary Health Network, the Hub provides access to a mental health professional who organises access to counselling, information and referrals based on the clients’ individual needs. We were able to quickly support a client who wasn’t even able to be put on a private psychologist’s waitlist due to overwhelming demand.
We’re proud to have a No Wrong Door approach meaning that all Victorians of any age who are experiencing emotional distress, mental ill-health and/or addiction can receive immediate help from HeadtoHelp, along with their families and carers. We take a holistic approach to mental health and our HeadtoHelp clinicians use a personalised approach to understand what’s going on for each individual client. They draw upon the broad range of services available and identify which ones best suit the needs, whether that’s within IPC Health or through our external partners.
The Hub provided intensive evidence based counselling for a parent who was frightened to leave the house. With no prior history, the client had developed anxiety and obsessive-compulsive disorder since the spread of COVID-19 and was afraid of catching the virus and passing it on to the children.
We’re also pleased to be able to provide free counselling to people without a Medicare card such as an international student in their 20s who wouldn’t have otherwise had care. The client’s mental health had deteriorated due to pandemic isolation and not being able to see their overseas family.
The IPC Health HeadtoHelp Hub model aims to normalise and encourage the treatment of minor mental health issues in the community before they affect clients’ day to day lives. By providing immediate and personalised support, we’re able to help move the community from intensive intervention to the prevention of mental ill health.
Accepted and have provided support to
Average of
IPC Health has invested in a complete refresh to modernise and mobilise the organisation’s technology, enabling staff to work in real time while continuing to deliver services to clients offsite
We’ve successfully rolled out the majority of the organisation wide Modern Workplace information and communications technology upgrade including new laptops, computers, telephony, software and shared platforms to give staff robust and reliable technology services. This has enabled us to be responsive to the new ways of working introduced by COVID-19 restrictions while exploring innovative ways to use technology for better client outcomes.
The Dental team have had a particularly interesting year again. When lockdown restrictions meant that they were only able to provide emergency services, the rest of the team were kept busy helping out in other areas of the organisation where they were needed most. Whether it was screening incoming clients at campus entries or getting hands on in the testing sites, they made a great difference to our community and staff were very grateful for the extra back up.
Still images from our advocacy campaign video for the Victorian Oral Health Alliance
Our Refugee Health Program works solely with people from a refugee background and people seeking asylum who live, work or study in the Brimbank, Hobsons Bay or Wyndham local government areas. For the majority of our clients, English can be a challenge and they prefer to see practitioners face to face. While the team adjusted to working from home, they also made continuity of care a priority working in collaboration with telephone interpreters.
Lola* is a mother of three children in her 50s. As a young child Lola and her family fled their country due to civil war and lived in a refugee camp for 20 years. Lola met and married her husband in the camp where the children were. After her husband died in his village, Lola and the children migrated to Australia as refugees.
Lola was referred to the Refugee Health program soon after her arrival. Since being involved in the program Lola has been referred to other IPC Health services including physiotherapy and dietetics. Lola has also been referred to other organisations such as the Foundation House to help manage the trauma she has suffered throughout her journey.
Our Refugee Health Nurse contacted Lola by phone with an interpreter for a general welfare call. During this conversation, Lola said that she had run out of medication and didn’t know how to make a GP appointment. She was also unsure how to make her way to the GP clinic on public transport as she had no private transport or friends or family to help her. The Refugee Health Nurse liaised with the Refugee Access Worker to arrange a GP appointment and for the Refugee Access Worker to meet Lola to support and teach her how to navigate the way to the GP independently.
A week after the GP appointment during another check in phone call, Lola said she was feeling very unwell with shortness of breath and chest pain. The Refugee Health Nurse called the ambulance while providing handover via phone to the paramedics. Lola was transferred to hospital where she remained for over a week. Our Refugee Health Nurse also informed Lola’s GP of her ambulance trip and subsequent hospitalisation ensuring they were kept updated.
Lola’s health has now improved and she is able to confidently attend her follow up appointments with the GP related to her recent hospital admission as well as other health issues. The services provided by the Refugee Health team not only attended to Lola’s urgent physical health needs but has also enabled her to manage her health needs more independently.
*Name changed to protect privacy
Our client Michael sustained significant injuries after a fall in August 2019 which resulted in a major decline in his ability to walk and complete his usual daily living activities. He commenced physiotherapy treatment with us in June 2020, at which point he was able to walk around 10 metres indoors with the use of a Zimmer frame but he was not confident to walk outdoors. Michael’s main goal was to be able to walk to the St Albans wetlands, a 200 metre walk from his house.
Despite the state wide lockdowns, we were able to maintain consistent physiotherapy home visit sessions which was complemented with telehealth exercise sessions with his exercise physiologist. After six months of strengthening exercises, Michael regained his confidence to achieve his goal of walking to and from the wetlands, something which he continues to do today.He is now also linked in with our Social Prescribing program who will work with him to find other suitable community-based activities that may further support his recovery journey.

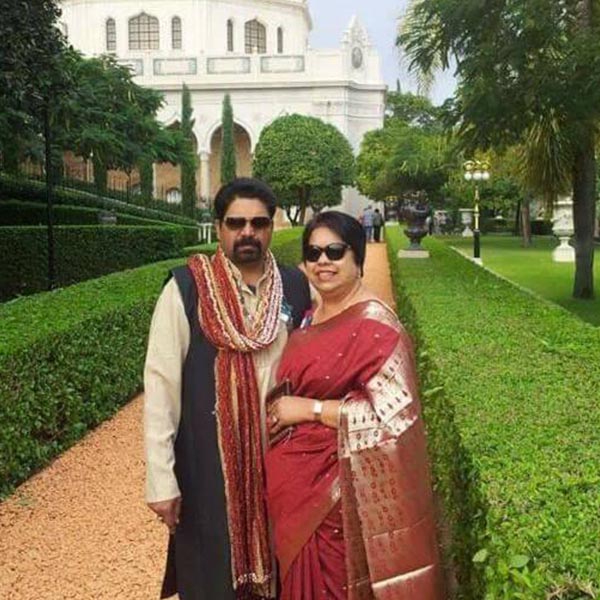
For the Sens, family really is everything. When setting up the interview for this story, interrupted by another lockdown, dad Randhir insisted that his two adult children were involved; daughter Raksha and son Manish because Randhir knew his kids’ place in telling the story of the family’s changing journey with IPC Health was an important one.
It’s been about a year since the family lost their beloved matriarch, wife and mother Vijay to complications of motor neurone disease (MND); you may have heard of it because of the Big Freeze event at the MCG and beanie appeal each year for FightMND, cofounded by AFL legend Neale Daniher. MND is currently incurable and attacks the body’s functions of independent movement, talking, swallowing and breathing. According to FightMND, the average life expectancy is just 27 months from diagnosis.
It all started with a sore shoulder and from there it was a difficult journey for Vijay through misdiagnosis and barrages of tests. When the final diagnosis of MND came back, they were shocked. “We’d never heard of MND so we did lots of research,” says Raksha. “But my aunt is a nurse so she knew exactly what it was and it was the news she was dreading.” It then came down to what could be done to improve Vijay’s quality of life.
Our employees are passionate and creative, we are One Team that strives to make a difference to the people and communities we serve. Our People Matters Survey highlights the passion we have for our work with 83% of respondents reporting they were proud of where they worked and would recommend IPC Health to prospective employees.


For the year ended 30 June 2021